Background
Presently, acute myeloid leukemia (AML) risk stratification is estimated prior to treatment by incorporating patient and disease characteristics. However, apart from the limited use of minimal residual disease measurement, few methodologies assess AML relapse risk post-treatment. In attempts to correlate pre- and post-treatment blood cell counts with hematologic disease outcomes, the ratio, LNR, between absolute lymphocyte count (ALC) and neutrophils (ANC) has been utilized to approximate the relationship between the lymphoid system and the myeloid microenvironment (in particular myeloid-derived suppressor cells), and increased LNR is prognostic in myeloma and lymphoma. Similarly, increased LMR (lymphocyte to monocyte ratio), utilized as a crude marker of tumor-infiltrating lymphocytes and tumor-associated macrophages, predicts better outcomes in Hodgkin's disease (Romano et al. Ann Hematol2018). However, analyses correlating such ratios with AML outcomes have not been performed. Here we specifically investigate whether LNR, LMR, or neutrophil-monocyte (NMR) ratios, measured at multiple time-points, correlate with outcomes.
Methods
We identified patients >18 yrs receiving induction chemotherapy at our institution between 1/1/2005 - 12/31/2019. Data collected included demographics, comorbidities (Charlson Comorbidity Index [CCI]), AML subtype, cytogenetics/molecular data, ELN risk stratification, and response to therapy. We recorded patients' total WBC, ANC, ALC and AMC both prior to treatment, at first ANC recovery (ANC > 1.0 x 109/L with ALC and AMC > 0), and just prior to next therapy. We also identified a subset of patients who received consolidation chemotherapies with curative intent and collected their first WBC counts ~100 days post-therapy completion (range 50-150 days). The calculated LNR, LMR, and NMR at these time-points were correlated with Event-Free Survival (EFS), defined as time to relapse, death from any cause, or last follow-up. Data was censored on 6/1/2020. WBC ratios were categorized into tertiles. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated using Cox proportional hazards models, survivor functions estimated using Kaplan-Meier and the equality of survivor functions tested using stratified log-rank tests. Outcomes were adjusted for CCI, age, sex, race, subtype, presence of inflammation/infection, and ELN risk.
Results
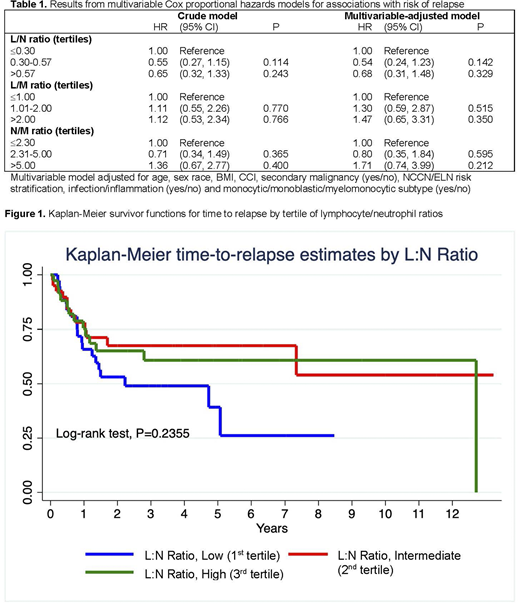
145 patients met eligibility criteria, however 23 with primary refractory AML were excluded from EFS analysis. Using WBC ratios at first ANC recovery, both intermediate and high LNR trended towards a lower HR for EFS: HR 0.54 (95% CI 0.24-1.23,p= 0.142) and 0.68 (95% CI 0.32-1.33,p= 0.329), respectively, however differences were not statistically significant (Table 1 and Figure 1). A high NMR also trended towards a worse EFS: HR 1.71 (95% CI 0.74-3.99,p= 0.212), though it was also not statistically significant. LMR did not correlate with improved EFS. Notably, pre-induction ratios and the ratios measured just prior to next treatment were not associated with any differences in EFS. In a subset of patients who received curative intent consolidation chemotherapies (generally ELN favorable risk), a t-test correlating for relapse was performed, though limited by small numbers (16 without, 8 with relapse). Patients in this group who did not relapse trended toward a numerically higher LNR and LMR, 0.57 vs 0.50 (p =0.36) and 4.33 vs 3.97 (p= 0.39), respectively.
Discussion
In our patient population, high LNR after induction chemotherapy trended towards predicting an improved EFS. Thus, recovery WBC ratios, although crude approximations of the immune system and the tumor microenvironment, may predict patients at higher risk of relapse, however, more patients are clearly needed to show whether a statistically significant association exists. The optimal time to evaluate these counts is also not clear. Nonetheless, as blood counts are obtained routinely post-treatment, these ratios may represent a low-cost strategy to predict relapse risk, potentially allowing for earlier treatment and donor searches for allogeneic transplantation. We propose to repeat these analyses using a multi-center approach - we are especially interested in ratios measured at the 100 days post-therapy mark, as we suspect these may better reflect the immune system at steady state and, potentially, risk of relapse.
Arain:Astellas:Other: Spouse is employed.Calip:Flatiron Health:Current Employment.Khan:Takeda:Research Funding;Celgene:Consultancy;Incyte:Honoraria;Amgen:Consultancy.Patel:Amgen:Consultancy;Janssen:Consultancy;Celgene:Consultancy.Quigley:Amgen:Other: Advisory board;Agios:Speakers Bureau;Alnylam:Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal